Abstract
Introduction High-dose chemotherapy and autologous stem cell transplantation (HDCT/ASCT) is widely used in diffuse-large B-cell lymphoma (DLBCL) patients. Since HDCT/ASCT in elderly patients is associated with increased morbidity, the clinical impact is not well defined. In addition, only very few data for HDCT/ASCT with reduced intensity conditioning in elderly DLBCL patients exists.
Methods We performed a single center retrospective analysis of 146 DLBCL patients aged 60 years and older who received HDCT/ASCT between 2005 and 2019. Statistical analyses were conducted with GraphPad Prism 5® and SAS V9.4.
Results Patients were analyzed according conditioning regimens: 86 patients received standard intensity high-dose conditioning (SI-group) with BEAM (BCNU, etoposide, cytarabine, melphalan) or TEAM (Thiotepa, etoposide, cytarabine, melphalan) and 60 patients received reduced intensity high-dose conditioning (RI-group) with BM (BCNU, melphalan, 43.3%), TM (Thiotepa, melphalan, 16.7%), BCNU/or Busulfan-Thiotepa (38.4%) or Bendamustin-melphalan (1.7%).
Comparing patients characteristics in the SI and RI-group, we found a difference for age (median age 65.5 vs. 71.8, p<0.001) and ECOG 0 vs ≥1 p=0.006, whereas we found no difference for other prognostic factors like disease stage, elevated LDH, extra-nodal disease or bulky disease. We found no statistical difference for remission status before ASCT (SI-group: PR/CR1 58.1%, PR/CR>1 25.6% and refractory disease (14%); RI-group: PR/CR1 41,7%, PR/CR>1 35% and refractory disease in 21.7% of patients), or lines of prior therapy (SI-group: 1 in 60.5% and ≥2 in 39.5% of patients, RI-group: 1 in 50% and ≥2 in 50% of patients).
We observed no significant difference in frequency or severity of relevant toxicities like febrile neutropenia, enterocolitis, sepsis, lung infections, mucositis or atrial fibrillation. Median time of hospitalization did not differ between both groups (15 vs. 17 days).
We found no difference for remission status after HDCT/ASCT between both groups. Cumulative incidence of relapse was higher in the RI-group: 30.8% (RI-group) and 23.4% (SI-group) at three years, p=0.034. We observed no difference in non-relapse mortality (NRM) 14.4% vs. 12.8% at three years.
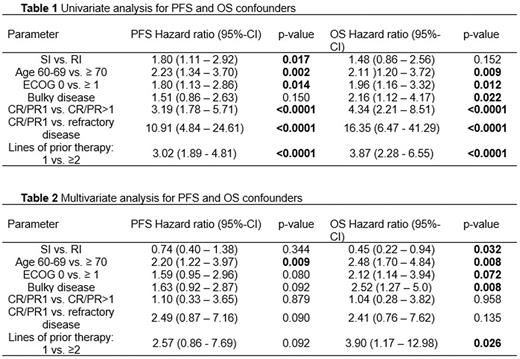
With a median follow-up of 62.4 month, we observed a 3-year overall survival (OS) of 67.1% and a 3-year PFS of 59.3%. Univariate analysis revealed several factors associated with inferior PFS and/or OS Table 1. Reduced intensity conditioning was associated with an inferior PFS, but not an inferior OS. Of note, in a multivariate Cox Regression analysis, we observed no difference in PFS (HR 0.74 (0.40 - 1.38) p=0.345), but a trend for better OS with reduced intensity conditioning (HR 0.45 (0.22 - 0.94) p=0.032) Table 2.
Conclusion: Reduced-intensity conditioning with two alkylating agents and omission of etoposide and cytarabine is feasible in elderly patients. Our retrospective analysis indicates a comparable outcome of SI and RI conditioning, when corrected for multiple significant confounders.
Disclosures
Finke:Riemser Pharma: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal